What is Hysteroscopy?
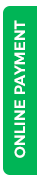
A hysteroscopy is a procedure to look inside the womb (uterus) to check and treat for any problems. A hysteroscopy is done with a narrow tube-like telescope (Hysteroscope) with a camera.
Who needs it (Indications) ?
Your doctor may advise you Hysteroscopy for any of the following reasons:
-
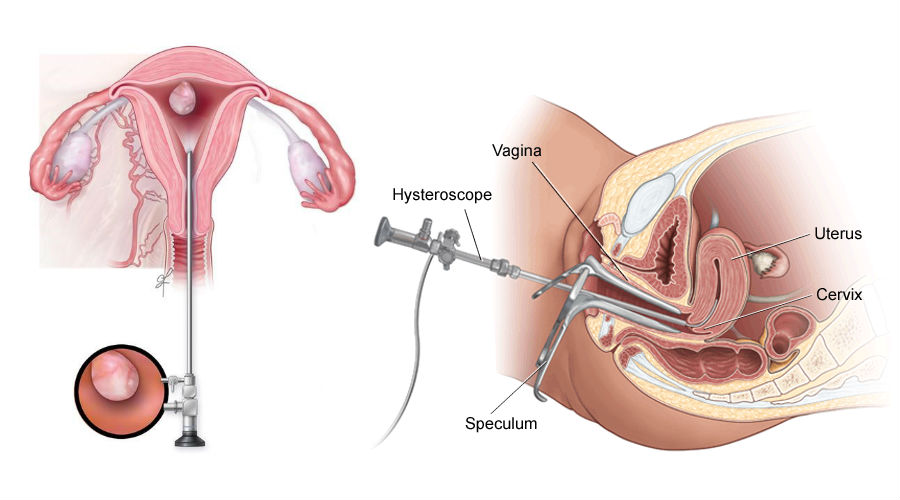
To find out what’s causing any unusual or abnormal vaginal bleeding. This can include heavy periods, bleeding between periods or bleeding after menopause
-
To diagnose the cause of Infertility or repeated Miscarriages
-
To remove polyps (small growths of tissue) and some types of fibroid (non-cancerous growths of muscle).
-
To remove scar tissue (adhesions) in the lining of your uterus
-
To find and remove displaced Intra-Uterine Devices (IUDs)
-
Incomplete evacuation following D &E : Retained products of conception (RPOC)
-
Guided endometrial biopsy to rule out cancer.
-
To correct birth defects like Septate or sub-septate uterus.
How to prepare for the procedure ?

1.
You will be scheduled to have the procedure after your periods and before ovulation. This lets your gynaecologist get the best view of the uterus. It also avoids harm to a new pregnancy.
2.
Your doctor will advise few basic blood tests to check your overall fitness for the procedure.
-
Tell your healthcare provider if you are sensitive to or are allergic to any medicines, iodine, latex, or anesthesia.
-
Tell your healthcare provider of all medicines (prescription and over-the-counter) and herbal supplements that you are taking.
-
Tell your doctor if you have a history of bleeding disorders or if you are taking any blood-thinning medicines (anticoagulants), aspirin, or other medicines that affect blood clotting. You may be told to stop these medicines before the procedure.
-
Follow any other instructions your provider gives you to get ready.
3.
You should be in a fasting state for at least six (6) hours before the procedure as it may be done under general anaesthesia.
4.
Sometimes the procedure might be done under local anaesthesia or no anaesthesia (Office Hysteroscopy). This depends on what other procedures your doctor will do at the same time and in selected cases.
5.
You will be asked to sign a consent form that gives permission to do the procedure. Read the form carefully and ask questions if something is not clear.
What happens during the procedure?

Hysteroscopy is usually done under general anaesthesia. This means you’ll be asleep during the operation.
The procedure usually takes about 10 to 15 minutes depending on what you are having it for but you will have to be under observation till the anaesthesia effect wears off.
You will be positioned on an operating table, lying on your back with your feet in stirrups.
The vaginal area will be cleaned with an antiseptic solution.
Your doctor may dilate your cervix before inserting the hysteroscope. With the 2.9 mm hysteroscope available at IHR there is usually no need to dilate the cervix which gives better comfort to our patients.
The hysteroscope is inserted into the vagina, through the cervix, and into the uterus.
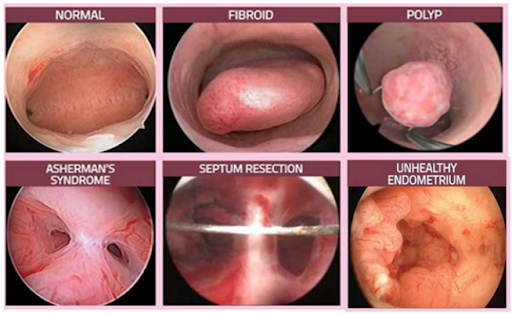
Sterile fluid, such as saline (salt) water, will be put through the hysteroscope into your uterus to expand it. The fluid helps your doctor to see the inside of uterus more clearly. The amount of fluid used is carefully checked throughout the procedure.
A camera on the hysteroscope sends pictures of the inside of your womb and the openings of the fallopian tubes to a monitor where your doctor can see it.
They’ll observe these images to find out the problem and will do the treatment that’s needed.
What to expect during recovery?

-
Hysteroscopy is most often done on an outpatient basis.You should be able to go home shortly after the procedure. If you had general anaesthesia, you may need to wait until its effects have worn off.
-
After a general anaesthetic, you may find you’re not so coordinated or that it’s difficult to think clearly. This should pass within 24 hours. In the meantime, don't drive, drink alcohol, operate machinery or sign anything important.
-
You might have some discomfort as the anaesthetic or painkiller wears off. You can take the prescribed pain medications if you need to.
-
It is also normal to have little bloody discharge from your vagina for a few days after the procedure.You can use sanitary pads until the bleeding stops – it’s best not to use tampons.
-
You can go back to normal activity and diet from the next day onwards unless your healthcare provider tells you otherwise.
-
You can usually exercise when any bleeding and pain has settled down.
-
It is advisable to avoid sex for a week or until any bleeding has stopped, to reduce the risk of infection.
What are the associated risks?
Most women don’t have any problems after having a hysteroscopy. But contact your doctor or visit the emergency department of your local hospital if you have:
-
Heavy bleeding
-
Signs of an infection, such as a fever, shivering and chills or foul-smelling discharge from your vagina
-
Severe abdominal (tummy) pain
There is a small risk of complications, and these are more likely to happen in women having operative rather than diagnostic procedures.
These complications, which are all very rare, include:
-
Damage to the womb: Treatment with antibiotics or, in rare cases, surgery may be required.
-
Damage to the cervix: This can usually be easily repaired if it occurs.
-
Womb infections: This can cause an odorous discharge, fever and heavy bleeding, and can usually be treated with a short course of antibiotics.
-
Feeling faint or dizzy: Around 1 in 200 women who have a hysteroscopy either under local anesthetic or with no anesthetic will feel faint.
-
Excessive bleeding during or after the procedure: This can be treated with medication or a further procedure. In very rare cases, the womb may need to be removed.
-
Complications from fluid used to expand the uterus.

.png) 0361-2800800
0361-2800800 (+91) 9864103333
(+91) 9864103333