What is a Semen Analysis?
It is a technique where we analyse your semen in lab to check the quality and quantity of the sperm. It is usually the first male fertility evaluation we do in the fertility assessment process.
It helps us to
Check the patency of the male genital.
Secretion of accessory organs.
Functional ability of the testis
What to expect during semen analysis ?
Getting a semen analysis may seem intimidating for many men and their partners, but there’s no need to feel embarrassed. 1-2 men fail to ejaculate ‘on demand’ in the clinic (Situational Anejaculation). There is no need to panic, inform your Doctor, there are ways to help you in such situation.
Male infertility is a common condition affecting 1 in 10 men.
In fact, up to 1 in 20 men have no sperm at all in their ejaculate. Even if you have no sperm in your ejaculate, this doesn’t mean you’ll never be able to have a child. We can help up to 70 percent of men who have no sperm at all (Azoospermia) in their ejaculate have children.
Why do it at IHR?
We follow strict and updated guidelines laid down in WHO laboratory manual for the examination and processing of human semen.
Have separate advance andrology lab
(see our infrastructure).
Have trained lab technician.
This helps us to properly evaluate your sample for correct assessment of your fertility and future plan of action. Many non-specialised labs do not follow these criterias and thus results in variations in the report and improper diagnosis.
What should I do before my appointment?
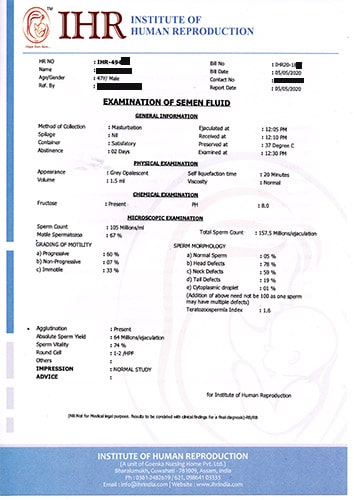
| Appearance | Homogenous Grey Opalascent |
| Volume | ≥ 1.5ml |
| pH | ≥ 7.2 |
| Self liquefication time | 20 to 30 minutes in room temperature |
| Sperm concentration | ≥ 15 X 106/ml |
| Total sperm count | ≥ 15 X 106/ejaculation. |
| Motility (PR + NP%) | 40% |
| Progressively Motility | 32% within 60 minutes of ejaculation |
| Morphology | ≥ 4% with normal form |
| Teratozoospermia Index | ≤ 1.6 |
| Vitality | ≥ 58% |
| Round cell | ≤ 5 millions/ml or 5 round cell/HPF |
| Pus cell | < 1 X 106/ml |
| Sperm yield |
> 5 million/ejaculation: IUI
2-5 million/ejaculation: IUI/IVF 1-2 million/ejaculation: IVF < 1 million/ejaculation: ICSI |
Motility Explained
Morphology Explained
What is covered in the report?
Physical Examination
-
Appearance:Looking for anything unusual to the naked eye.
-
Volume:Amount of semen produced and for a normal sample this needs to be more than 1.5 ml.
-
Self-Liquefaction time:Time taken for the sample to change from a thick gel into a liquid(20-30 mins normally).
-
Viscosity:This means being thick, sticky, and semifluid in consistency. The ideal is normal, but it could also be classed as highly viscous or slightly viscous.
Chemical Examination
-
pH:This refers to how acidic or alkaline the semen is. Semen is ideally between 7.2 and 8 which makes it slightly alkaline.
-
Fructose:
Presence or absence of fructose
Microscopic Examination
-
Sperm count:
Concentration of sperm/ml. -
Total sperm count:
Total sperm count/ejaculation. -
Grading of motility:
Assessing movement of the sperm. -
Sperm Morphology:
Assessing structure of the sperm -
Teratozoospermia index (TZI) :It is a measure of the average number of defects per spermatozoa, which could be used to improve the correlation between sperm morphology and fertility.
-
Agglutination:
This refers to stickiness - what percentage is clumping together. -
Absolute sperm yield:
Total number of progressively motile sperm/ejaculation. -
Sperm Vitality:
Percentage of live sperm/ejaculation -
Round Cells:
These may be signs of infection, if there are more than 1 million cells per ml.
Results
-
Normal study
-
Aspermia:
absence of semen -
Azoospermia:
absence of sperm -
Hypospermia:
low semen volume -
Hyperspermia:
high semen volume -
Oligozoospermia:
very low sperm count -
Asthenozoospermia:
poor sperm motility -
Teratozoospermia:sperm carry more morphological defects than usual
-
Necrozoospermia:
all sperm in the ejaculate is dead -
Leucospermia:
a high level of white blood cells in semen

.png) 0361-2800800
0361-2800800 (+91) 9864103333
(+91) 9864103333